Male Fertility
Overview
This section highlights the common questions and concerns about fertility potential, becoming a father, sperm retrieval options, and changes in sperm quality after SCI.
MYTH
If I can’t ejaculate, I guess I’ll never have kids.
FACT
There are other options available to become a father.
What Is It?
Male fertility is defined as the ability to father a child.
How does Sperm and Ejaculation work?
- Sperm production starts with the release of hormones (LH and FSH) from the brain. These hormones send messages to the testes to produce testosterone and sperm
- Sperm matures in a 3 month cycle
- Ejaculation is typically how semen (which contains sperm) comes out of the body
- Ejaculation occurs in 2 phases:
- The first phase is called emission or “the loading phase”. During this phase sperm is released from the testicle and mixed with several fluids from different glands, the prostate, and seminal vesicles.
- The second phase is ejaculation proper or the “propulsion phase”. This is when the seminal fluid leaves the body through the urethra. This release can vary in speed, volume, or amount of ejaculatory fluid.
- Semen quality is assessed by looking at how many sperm are present (sperm concentration), what they look like (sperm morphology: i.e. size and shape of their head, body and tail), and what percentage are swimming and moving (sperm motility).
- Even though ejaculation and orgasm often happen together, they are separate processes and one can happen without the other.
FUN FACT
Did you know that the sperm that a man ejaculates today was made three months ago? If he was sick or had an infection then, the sperm today may be of lesser quality!
What’s Different Now?
Following spinal cord injury there is a change in the communication system between the nerves, muscles, spinal cord, and brain. This disruption in the communication system can negatively affect a man’s ability to ejaculate.
If you have a complete SCI, chances are the ability to ejaculate will be quite low. If your injury is above T10 (a higher level injury), there is a greater possibility that ejaculation can occur with the use of specialized devices (discussed in more detail in the next section). Lower injuries often require more invasive options.
If you have an incomplete SCI, the ability to ejaculate is difficult to predict and it is often unreliable. This is due to messages being sent from the brain that can interrupt the reflex.
What Can I Do About It?
Explore! Do this with curiosity, but be cautious about your blood pressure getting too high (AD). Also be aware that if you are trying too hard to ejaculate and this is your main goal, it can lead to frustration. If you are having difficulties and would like to learn more about sperm retrieval options, contact the Sexual Health Rehabilitation Service.
Sperm Retrieval Options:

Vibrostimulation Reflex Arc
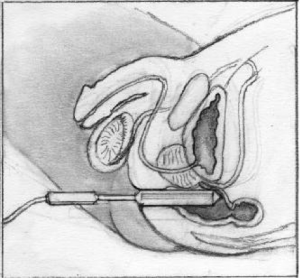
Vibrostimulation: A procedure where a specialized vibrator (that doesn’t look like a penis, just in case that thought crossed your mind!) is applied to the head of the penis to attempt to provoke ejaculation. The vibrators used for this procedure need to be more powerful than ones you would typically find at a sex shop. This is because more stimulation is needed on the penis for your spinal cord to get the message that ejaculation can occur. This procedure is most successful in men with complete injuries above T10. See diagram.

An example of an electroejaculation vibration device. Learn more in the Spin Doctor Article on male fertility questions.
 Electroejaculation: is a procedure that is used when vibrostimulation fails. It is most commonly used for sperm retrieval when the spinal cord injury is below T10. This procedure can occur either in the clinic (i.e. if there is no anal sensation: complete injury) or in the operating room (i.e. when anal sensation is present; incomplete injury). This procedure involves the insertion of a foley catheter that blocks the bladder neck so seminal fluid comes forward out of the penis, rather than back into the bladder. A rectal probe, delivers an electrical current to the prostate through the rectum. This procedure is quite effective in producing an ejaculate for reproductive purposes.
Electroejaculation: is a procedure that is used when vibrostimulation fails. It is most commonly used for sperm retrieval when the spinal cord injury is below T10. This procedure can occur either in the clinic (i.e. if there is no anal sensation: complete injury) or in the operating room (i.e. when anal sensation is present; incomplete injury). This procedure involves the insertion of a foley catheter that blocks the bladder neck so seminal fluid comes forward out of the penis, rather than back into the bladder. A rectal probe, delivers an electrical current to the prostate through the rectum. This procedure is quite effective in producing an ejaculate for reproductive purposes.
MYTH
Poor semen quality in men with SCI is due to higher scrotal temperatures from sitting.
FACT
There has been no published reports that this is true—attempting to cool your nether regions will be a futile effort!
Have questions about male fertility or sperm retrieval after spinal cord injury?
At the Vancouver Sperm Retrieval Clinic, we are experts on male fertility and sexual health after spinal cord injury, damage to the nerves in the pelvic area, or other conditions which may interfere with the ability to ejaculate. We also see men with ejaculatory difficulties who are actively trying to conceive.
Surgical Sperm Retrieval: Sometimes, when vibrostimulation and electroejaculation have been tried and the results have been poor (little to no sperm), surgical sperm retrieval is attempted. This procedure is done by placing a needle into the testicle or surrounding structures to remove sperm cells. The number of sperm cells retrieved by this procedure is considerably less than other methods. The image beside highlights the structures that sperm can be extracted from.
Semen Quality: We know that semen quality changes post SCI. This has to do with changes to the seminal fluid, however, the exact causes for these changes are still being researched. Typically, men with SCI have good sperm concentration (number of sperm), however, sperm motility (the amount the sperm move/swim) and what they look like (morphology) are most commonly affected. Your semen quality and quantity will determine what insemination option is most suitable for you.
Insemination Options:
Intravaginal insemination (IVI) AKA, the “turkey baster method”: this technique is where ejaculated semen is drawn up into a needless syringe and placed directly into the vagina. This technique is typically done in the home setting. Please see the “tips for home insemination” info sheet on the side bar.
Intrauterine insemination (IUI): This method is done at a fertility clinic. This procedure can be done with either fresh or frozen semen. It requires at least 5 million motile sperm per insemination. In this procedure, the sperm is washed and separated from the semen by an andrologist (a sperm specialist). This is a process that the cervical opening would typically do. Once the sperm is washed it is put directly into the uterus through a small catheter.
In- Vitro Fertilization (IVF): This is a more complex procedure requiring medications and more advanced interventions at a fertility clinic. In this procedure, a woman is given medications to get her body to mature many eggs at once (not just one or two her body would typically do on its own). She is monitored with ultrasound and when they are ready, the eggs or oocytes are then retrieved from her ovaries. For this procedure eggs and sperm (multiples of each) are place in a petri dish to fertilize on their own. The successfully fertilized eggs are then incubated for 3-5 days to become embryos. At that time the embryo quality is determined and plans for transfer or freezing are made.
Intracytoplasmic Sperm injection (ICSI): This is similar to IVF in its complexity. Egg retrieval is done the same as explained above. The main difference is how the sperm fertilizes the egg. In this process, one sperm is injected directly into each egg. This is done typically when sperm counts are lower, the shape of the sperm (morphology) is abnormal or when the sperm is taken directly out of the testicle (sperm aspiration). The successfully fertilized eggs are then incubated for 3-5 days to become embryos. At that time the embryo quality is determined and plans for transfer or freezing are made.
Embryo transfer: Embryo transfer is the last step in either the IVF or ICSI process. It is where the embryo (either fresh or frozen) is placed back into the uterus using a small catheter and ultrasound. A pregnancy occurs when this embryo implants to the uterus wall. This can be determined by a blood test 10-14 days after the transfer.
What Do I Need To Know?
It is important to know the resources in your local area. A consultation with a medical professional before trying something like vibrostimulation (VS) is strongly recommended. Autonomic dysreflexia (AD) commonly occurs with vibrostimulation, therefore, it is not recommended VS be done at home without medical advice.
It is also important to know sperm retrieval is the first step in determining your fertility potential. Once sperm is obtained, it needs to be sent to a lab for an analysis to determine semen quality. The quality of sperm will determine the most appropriate method for insemination (aka baby making!)
FUN FACT
There have been over 200 babies born in the last 30 years of the Vancouver Sperm Retrieval Clinic!
My Role
Equip yourself with the information provided in this chapter and understand your own injury. Even if you aren’t ready for to start a family right now, this information can give you direction when you are ready. This information may also be helpful when discussing future plans with a partner.
Who Can Help Me?
Clinicians at the Vancouver Sperm Retrieval clinic, or if you are not located in B.C., please click here for a list of practitioners within Canada who may be able to assist you.
Head to our contact form and get in touch with us if you are not close to a Canadian sperm retrieval clinician.
Conclusion
Despite changes to ejaculation after SCI, becoming a father is still possible. Being familiar with the resources and options available to you can be important when you decide you would like to start a family. It is common for men to want to understand their fertility potential even before they are in a relationship. You can start this process at any time, even if you aren’t planning to start a family right away. Knowing your options, and knowing your body now, is a great way to feel more sexually confident.
Male Fertility Resources
Articles and Other Resources
Male Fertility After Spinal Cord Injury: A Guide for Patients (PDF) - Miami Project to Cure Paralysis.
Spin Doctor Article on male fertility questions with Shea Hocaloski, Sexual Health Clinician, Vancouver Coastal Health.
Videos
Dr. Stacy Elliott of SHRS Demonstrates the Ferticare Vibrator - ICORD.
Dr. Stacy Elliott of SHRS Talks Vibrostimulation - ICORD.
Principles for Sexual Health Rehabilitation with Dr. Stacy Elliott - SCI Canada.
Things to Consider in Male Fertility After SCI - Facing Disability.
Fertility - Sexuality After SCI
Check out the Video Playlist for this chapter.

